Launching 1st March 2023. Also check out: https://www.thailandmedical.news/
Human papilloma virus (HPV) infection of the uterine cervix can lead to cervical cancer in a small percentage of cases. HPV infection is usually cleared from the body by the immune system within approximately two years. Persistent or recurrent infection may lead to the development of cervical cancer.
Cervical cancer is the fourth most frequent cancer in woman. In 2012 there were about 530,000 new cases of cervical cancer globally. It accounts for about 270,000 deaths each year, which comes to around 7.5% of all female cancer deaths. In the UK, for example, over 3000 women are diagnosed with this cancer each year. However, the majority of patients with the disease, namely 85%, come from less developed countries. The global mortality rate for cervical cancer is high at 52%.
Cervical cancer is not a hereditary disease. The cancer develops as a consequence of HPV infection, following the transmission of oncogenic strains of the virus. This may occur through skin-to-skin contact in the genital areas of the vagina, anus or through the mouth or throat.
Cervical cancer can take several years to become established. In general, it takes about 15-30 years for the cancer to develop in an individual with a robust immune system. If the immune status is compromised, as in a person with HIV infection, for example, this time may be as short as 5-10 years. It is the most common cancer in women under the age of 35
Other risk factors for the disease include:
HPV infection leads to the takeover of the epithelial cell by the virus, with expression of two proteins called E6 and E7. These interfere with the normal cell regulatory functions, leading to uncontrolled cell proliferation and inhibition of programmed cell death (apoptosis) at the end of its life cycle. Usually, such infected cells are removed by the immune system. If not, persistent infection leads to mutations in the cellular genes which promote greater proliferation. The end-result is precancerous changes, and finally frank cancer.
A dozen strains of HPV have been identified to be associated with future cervical cancer risk. Almost all cervical cancers have been found to follow HPV infection. However, about 70% of all cervical cancers are caused by HPV types 16 and 18. Two vaccines have been developed to protect against infection by these particular strains. One of the vaccines also protect against some forms of warts which develop through infection with types 6 and 11. These vaccines are most effective when administered at the age of 11-12 years to girls who have not yet engaged in sexual intercourse of any kind.
In the early stages there are no real signs of the disease. As the disease progresses symptoms appear, such as:
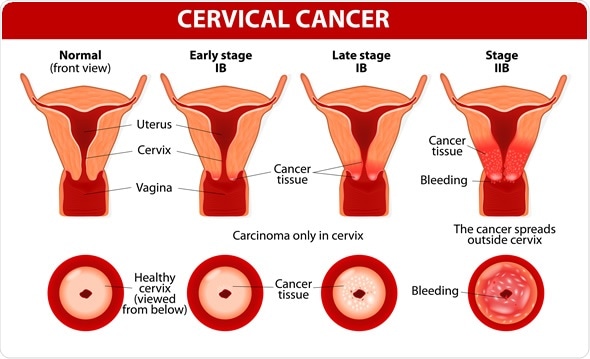
The cervix is the slim section which makes up the opening of the uterus into the vagina, or birth canal.
Cervical cancer forms when an oncogenic HPV virus transforms cells in the cervix into abnormal cells by inducing alterations to their deoxyribonucleic acid (DNA) or ribonucleic acid (RNA). The ectocervix is the part of the cervix which faces the vagina. It is lined by a layer of epithelium. It is continuous with the cervical canal, lined by glandular epithelial cells. This is also called the endocervix. The meeting point between the ectocervical and endocervical cells is called the transformation zone. Cells in this transformation zone are most likely to become cancerous.
When cervical cancer screening is carried out, professionals examine cells retrieved from the ectocervix through a smear test for suspicious changes in them. If there are mild signs of abnormality, the patient is advised to come in for regular monitoring. If more severe abnormalities are detected, the patient may be advised to undergo a colposcopy where the cervix can be visually and microscopically analyzed to identify the type and severity of the lesion, whether benign, precancerous or cancerous.
The three tests commonly used for cervical cancer screening include:
HPV testing in cervical cancer screening is indicated for: