Launching 1st March 2023. Also check out: https://www.thailandmedical.news/
Rheumatoid arthritis (RA) is a systemic disease of the immune system. It affects multiple joints in the upper and well as the lower limbs. Knees are one of the common joints affected by RA. RA can occur at any age and can affect both knees.
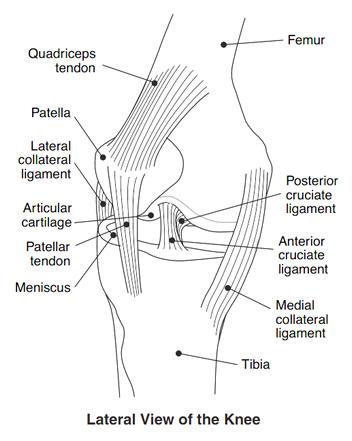
When RA affects the knee joint the synovium that lines the ends of the bones in the joints thickens and produces an excess of joint fluid.
This excess fluid, along with inflammatory chemicals that the immune system releases, leads to swelling and damage to the cartilage that acts as a cushion within the joint leading to pain, and joint erosion.
The symptoms most commonly include pain and stiffness of the affected joints. The pain is more often than not worse in the mornings associated with severe stiffness. The joint may become stiff and swollen, making it difficult to bend or straighten the knee.
Pain and stiffness is also at its worst after a period of inactivity. The knee may feel weak or may feel “locked” or may “buckle” as a result of this disease.
The diagnosis of RA affecting the knees is based on the same principles as diagnosis of rheumatoid arthritis of other joints.
The diagnosis is initiated with a detailed history of the onset and severity of the symptoms as well as family history of rheumatoid arthritis or other autoimmune disorders.
The next step involves physical examination where the affected and other joints are examined for swelling, pain and signs of inflammation. The range of movement of the knees, the pain, tenderness and the stiffness is noted.
There are several patient based questionnaires and measures called health assessment questionnaires (HAQ) that measure patient disability and quality of life. In addition these questionnaires also measure the patient’s own perception of the disease burden.
There are batteries of tests that may be employed in the diagnosis, however, none of these are definitive.
Due to inflammation blood tests such as C Reactive protein and Erythrocyte sedimentation rate (ESR) may be raised. These are, however, non specific markers of inflammation.
Rheumatoid factor is a relatively specific test. There is presence of this indicative factor in nearly 80% of all persons with rheumatoid arthritis. Presence of rheumatoid factor may not be detected in early stages of the disease. In addition, around 1 in 20 healthy persons may test positive for rheumatoid factor. Thus presence of rheumatoid factor is not absolutely indicative of rheumatoid arthritis.
Several imaging studies like X rays, MRI scans and CT scans may be ordered to look at the extent of joint damage caused by the disease. X-rays typically show a loss of joint space in the affected knee.
The aims of treatment are twofold: to relieve the symptoms of the disease and to prevent the disease progression and joint damage.
To ease the symptoms, pain relievers and anti-inflammatory agents are the primary mode of therapy. Non-steroidal anti-inflammatory drugs (NSAIDs) are the drugs used widely to control symptoms of rheumatoid arthritis. They are, however, notorious for their side effects due to which they may be used for short term basis only.
To prevent progression of joint damage Disease-modifying anti-rheumatic drugs or DMARDs are widely used. These agents have a varied mechanism of action and they act by reducing joint swelling and pain, decreasing markers of acute inflammation in blood and halt the progressive joint damage.
DMARDs include Methotrexate, Sulfasalazine, Leflunomide, Hydroxychloroquine, Gold salts and Ciclosporin. DMARDs however are also associated with a varying degree of side effects.
Corticosteroids are anti-inflammatory agents. They may be given as medications or as injections directly into the joint spaces in order to reduce the joint inflammation.
A newer approach is to use biological agents. TNF inhibitors were the first licensed biological agents including etanercept, infliximab, adalimumab and certolizumab. This was followed by monoclonal antibodies like abatacept, rituximab, and tocilizumab.
Supportive treatment includes exercise, joint protection, psychological support to help deal with the associated symptoms and disability.
Lifestyle modifications include losing weight and changing exercises from running or jumping exercises to swimming or cycling that do not carry the risk of damaging the knees. Weight loss can reduce stress on weight bearing joints, such as the knee.
Physiotherapy is an important part of therapy of debilitating arthritis. This helps maintain optimum joint flexibility and strength.
Assistive devices, such as a cane, walker, long shoehorn etc. may help cope with disability associated with knee rheumatoid arthritis.
Surgery may be performed to retain joint function or prevent loss of joint function. Joint replacement therapy may be chosen. This is vital when joints fail.
There are different types of surgery to correct joint problems. Total or partial knee replacement is often recommended for patients with rheumatoid arthritis.