Launching 1st March 2023. Also check out: https://www.thailandmedical.news/
Pneumocystis pneumonia is a condition caused by a microorganism called Pneumocystis jiroveci. This has been reclassified in recent years as a fungus due to its characteristic nucleotide sequences and cell wall composition. This type of pneumonia is mostly seen in immunocompromised patients, such as those with acquired immunodeficiency disorder (or AIDS).
Recent advances in the prophylaxis, diagnosis and treatment of Pneumocystis pneumonia have resulted in a decrease in associated morbidity and mortality. However, the disease continues to be an important clinical entity in patients with severe immunosuppression or whose adherence to specific prophylactic regimens is inadequate.
Pneumocystis jiroveci reproduces in association with the alveolar type 1 lining cell of the pulmonary tissue. For this reason, active disease is restricted to the lungs. If the ensuing pathological process is not limited by host immune activity or appropriate antimicrobial therapy, the affected alveoli will eventually be filled with this microorganism, along with proteinaceous fluid.
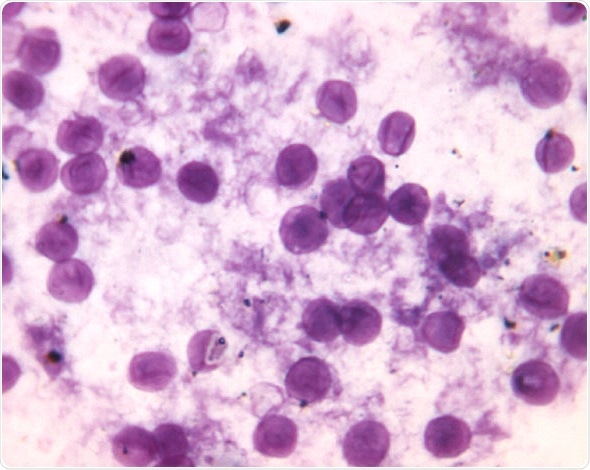
The classic lesion of Pneumocystis pneumonia is, therefore, an interstitial infiltrate of plasma cells and lymphocytes, as well as hyperplasia of specific pneumocytes. Furthermore, the alveoli are full of a characteristic foamy exudate, while the organisms appear as tiny bubbles in a background of proteinaceous fluid.
Such progressive filling of alveoli prevents adequate gas exchange, so the patient slowly suffocates. It can also lead to thickening of the interstitium of the lungs and potentially lung fibrosis. Owing to this mechanism of pathogenesis and its unique life cycle, Pneumocystis jiroveci cannot be cultured routinely, but is rather diagnosed by specific staining demonstrating the trophozoite or the cyst wall.
The classic triad of symptoms associated with Pneumocystis pneumonia comprises fever, nonproductive cough, and progressive exertional dyspnea. These are noted in only about 50 percent of cases. In other words, the signs and symptoms of the disease can be very subtle. This means that in order to establish a correct diagnosis it is necessary to have a high index of clinical suspicion and heightened awareness. This is especially so because the risk factors for HIV and other immunosuppressed situations may be denied or unknown.
Other symptoms associated with this type of pneumonia may include chills, weight loss, nonspecific chest discomfort. In rare instances the patient may have hemoptysis (coughing up of lood). If present, these symptoms usually show progress slowly over weeks to months. A careful medical history often reveals progressive, longstanding exertional dyspnea.
Physical findings on examination are also nonspecific. During auscultation fine dry crackles and rales are sometimes heard, but normal findings are observed in up to half of affected individuals. In children with severe clinical presentations, the findings may include nasal flaring, cyanosis and the retraction (inward movement) of rib muscles.
Extrapulmonary diseases caused by Pneumocystis jiroveci are rarely seen, but have been described in the medical literature. They occur especially in patients with advanced HIV infection without prophylaxis. They are known to involve organs such as the skin, spleen, heart, eyes or thyroid gland. Such presentations can occur even in the absence of lung disease.
A grave potential complication of Pneumocystis pneumonia is a pulmonary crisis akin to acute respiratory distress syndrome (ARDS) which may necessitate intubation. This happens infrequently, and leaves physicians faced with the dilemma of choosing between differential diagnoses of Pneumocystis pneumonia, classical bacterial pneumonia, tuberculosis of the lungs, as well as a myriad of other respiratory disorders.