Launching 1st March 2023. Also check out: https://www.thailandmedical.news/
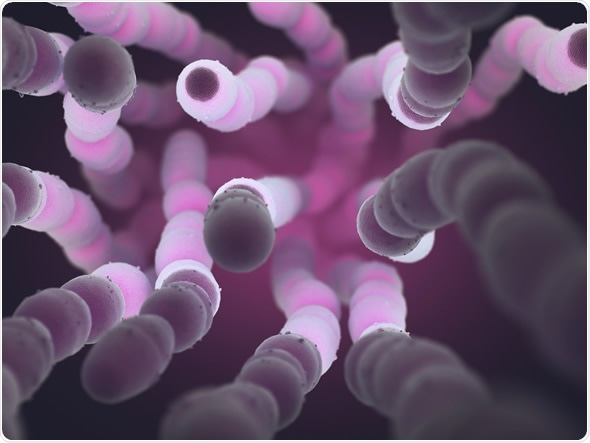
Streptococcus pneumoniae (pneumococcus) is a Gram-positive bacterium that is responsible for the majority of community-acquired pneumonia. It is a commensal organism in the human respiratory tract, meaning that it benefits from the human body, without harming it. However, infection by pneumococcus may be dangerous, causing not only pneumonia, but also bronchitis, otitis media, septicemia, and meningitis.
S. pneumoniae is alpha-hemolytic, meaning that it can break down red blood cells through the production of hydrogen peroxide (H2O2). The production of H2O2 by the bacterial infection can also cause damage to DNA, and kill cells within the lungs. Pneumococcal pneumonia causes fever and chills, coughs, difficulty breathing, and chest pain. If the infection spreads to the brain and spinal cord, it can cause pneumococcal meningitis, characterised by a stiff neck, fever, confusion, and headaches.
Pneumococcal infection is responsible for 1-2 million infant deaths worldwide, every year. During influenza epidemics, S. pneumoniae is associated with higher mortality in patients infected with both microorganisms. It is thought that S. pneumoniae and Haemophilius influenzae have a synergistic effect on one another, when infecting the same host.
The primary risk factors for infection are:
S. pneumoniae can be readily identified by culturing bacterial samples on blood agar. Due to the hemolytic properties of the bacteria, they will turn blood agar to dark green. However, growing bacterial cultures can take time. Therefore, it is more efficient to diagnose an infection using more modern techniques.
The first technique involves the detection of parts of streptococcus bacterium, known as antigens, in urine. C polysaccharide, a main component of the bacterial cell wall, can be detected in a number of bodily fluids. Immunochromatography is used to test for the presence of specific antigens, and compares favorably to diagnosis via bacterial culture.
The second technique involves an assay based on detection of S. pneumoniae-specific DNA sequences. These can be performed extremely quickly, and the high specificity conferred by using DNA as a target minimizes the risk of error.
Antibiotics are the first line of treatment for bacterial infections, and are effective against pneumococcus. However, treatment of pneumococcal infections is dependent on the strain that a patient is infected with. Some strains of S. pneumoniae have acquired a resistance to specific antibiotics, and therefore cannot be reliably treated with them. During diagnosis, cases of S. pneumoniae will often be tested for susceptibility to antibiotics, and the physician will make a judgement of treatment course based on the findings.
Prevention is considered to be better than a cure, and therefore vaccination is preferable to having to treat a disease. Two vaccines for pneumococcal infection are available, and both work on the same mechanism: delivery of antigens to provoke an immune response in the recipient. However, since the introduction of these vaccines to combat the spread of S. pneumoniae, some strains have been observed that do not carry the antigens that the body has been sensitized to. Other vaccine approaches are being considered, looking for antigens that are more readily conserved between bacterial strains.